Disclosure
Commercial support for this program has been provided by Michael Foods.
Looking to sign up for our newsletter? Click here
Sign up for NewsletterSauces & Dressings
Baked Goods
Pastas
Sports Nutrition
Pet Foods
Learn about our team’s extensive capabilities and resources.
Get to Know UsEggs
Potatoes
French Toast
See the Story From Our Farm To Your Table

Michael Foods Online CE Course (1 hour CE)
Michael Foods, Inc. will maintain verification of your attendance. Please fill out the following information. Upon completion of this course, a certificate of completion will be available for download.
Commercial support for this program has been provided by Michael Foods.

In the U.S., food allergy affects approximately 8% of children and 11% of adults, according to the National Institute of Allergy and Infectious Diseases (March 8, 2023). This translates into about 1 in 10 adults and 1 in 13 children (FARE, 2024).
Experts estimate that every year, food allergy is responsible for 3.4 million emergency room visits, 2,000 hospitalizations, and 150 deaths (FDA, 2023; USDA, 2024). FARE adds, “Every 10 seconds, food allergy sends a patient to the emergency room” (Facts and Statistics, 2024).
The majority of food allergies are diagnosed in childhood, says FARE. However, 15% of people with food allergies were diagnosed in adulthood. Just over half (51%) of adults and 40% of children who have food allergy have experienced a severe reaction, they say.
Food allergies can affect quality of life. Iglesia et al. (2024) speak to “the vigilance needed to avoid food allergens,” noting that it can cause “a significant impairment in the quality of life for both patients and caregiver”.

After completing this course, participants will be able to:
List at least three allergen-related topics to address in foodservice training.

Food allergy is an overreaction of the body’s immune system to a specific protein (an allergen) in a food, explains the American Academy of Allergy Asthma & Immunology (AAAAI, Food Allergy, 2024). When food allergy is present, a person may react to even a very small amount of the food. While food allergy is often diagnosed in childhood, they say, it can also first appear in older children and adults.
Developing a food allergy starts with sensitization. Upon exposure to the allergen, the body produces immunoglobulin E (IgE) antibodies. Essentially, the body is identifying the allergenic protein as an invader. The IgE antibodies attach to cells in the skin, lungs, and gastrointestinal tract. “If you come in contact with the allergen again, the cells release chemicals including histamine, which cause food allergy symptoms,” as explained by AAAAI (Food Allergy, 2024). “Each type of IgE has a specific ‘radar’ for each type of allergen” (AAAAI, Food Intolerance vs. Food Allergy, 2023). This response triggers the symptoms of allergy. Why some people become sensitized to a particular food allergen while others do not, is not understood (Iglesia et al., 2024).
Also, some people may have IgE antibodies to specific food allergens but do not show clinical symptoms of food allergy. This also is not understood, note Iglesia et al. They suggest that some factors that may play a role in development of food allergy are “genetic susceptibility, microbiome alterations, skin exposure to detergents, and pollutant exposure”. Having eczema in infancy is “the strongest risk factor for food allergies,” they add.
Food allergies are usually diagnosed through skin prick testing in the blood, as part of a consultation with a qualified allergist, says AAAAI. A clinician may also test for IgE antibodies, and the clinician interprets results in the context of a clinical history. Other approaches to identifying a food allergy include an elimination diet, which involves omitting a suspect food for a defined period of time and then reintroducing it; and an oral food challenge, which involves administering a suspect food in a safe, clinical setting and observing the response (Gargano et al., 2021).
Because food allergy is currently considered incurable, the treatment is an avoidance diet—avoiding the food that causes allergic reactions. This can be more difficult than it sounds. Iglesia et al. (2024) explain that people who are managing food allergies need to develop “food label literacy” to identify allergenic ingredients. They also need to develop the communication skills “to discuss food allergies with families, schools, restaurant workers, and food vendors.”
Explains AAAAI, some allergens may become less potent when treated with heat, which can change the nature of proteins. They comment, “Research is showing that more than half of children with milk and egg allergies can tolerate extensively heated milk and egg in baked foods” (Food Allergy, 2024).
Some children outgrow food allergies. This is most common for allergies to milk, egg, wheat and soy. In contrast, allergies to peanuts, tree nuts, fish, and shellfish “are generally lifelong,” according to the FARE (Facts and Statistics, 2024).

Typical symptoms of food allergy usually arise within two hours and can range from mild to severe, says the FDA (2023). Symptoms may be flushed skin, hives, itchiness, or swelling of the skin, abdominal cramps, vomiting, diarrhea, coughing, or wheezing. There can also be respiratory symptoms in conjunction with any of these other responses, says the AAAAI (Food Intolerance vs. Food Allergy, 2023).
A person can respond to even microscopic amounts of a food allergen. Even touching a food or inhaling an airborne allergen can trigger a reaction for some people, says the AAAAI.
Life-threatening anaphylaxis can involve severe difficulty breathing and shock. This “a serious allergic reaction that happens very quickly,” says the AAAAI. The immediate symptoms are swelling of the throat and vocal cords, difficulty breathing, dizziness, and/or or loss of consciousness. They add, “Without immediate treatment—an injection of epinephrine (adrenalin) and expert care—anaphylaxis can be fatal.”
The highest risk of a severe or fatal reaction occurs among teenagers and young adults, says FARE (Facts and Statistics, 2024). What’s more, “approximately 20-25 percent of epinephrine administrations in schools involve individuals whose allergy was unknown at the time of the reaction,” they note.
In rare instances, an infant may develop a condition called Food Protein-Induced Enterocolitis Syndrome (FPIES), says the AAAAI (Food Protein-Induced Enterocolitis Syndrome, 2023). Most common reactions are to milk, soy, or grain. The serious reaction causes vomiting and diarrhea and can lead to dehydration and shock, says the AAAAI. Rather than involving IgE antibodies, the reaction seems to involve the immune system cells, they explain.

So far, there is no cure for food allergies. Thus, the protocol is to avoid foods that trigger allergic responses.
Nevertheless, there have been some advances in treatment of food allergy, such as a treatment approach called allergen immunotherapy. This is “an intervention by which an allergic individual is exposed to initially small, gradually increasing quantities of the specific allergen responsible for clinical presentations,” explain Gargano and colleagues (2021).
In 2020, the FDA approved a allergen immunotherapy drug called Palforzia to reduce the impact of peanut allergy in children aged 4-17. It does this by “by allowing the immune system to build up a tolerance to peanuts over time,” explains Reardon (2024). Taken on an ongoing basis, the drug is intended to mitigate severe allergic responses and reduce the risk of life-threatening anaphylaxis for allergic individuals who consume peanuts (FDA, 2020). It is by no means a cure. Children who are taking the drug still need to avoid peanuts and carry epinephrine, says the FDA.
The National Institute of Allergy and Infectious Diseases (2023) describes food allergy research as an ongoing priority. In one recent study (2024), they reported that giving children a 16-week course of a monoclonal antibody called omalizumab increased the tolerance of a variety of allergenic foods.
Monoclonal antibodies are immune system proteins that are created in the lab. They are used in a variety of medical treatments. One way they can work in the context of food allergy is by binding with IgE molecules to make them less effective in triggering an allergic response. Omalizumab has been FDA-approved for asthma treatment since 2003, says Reardon, and it was approved for food allergy treatment in February, 2024 (FDA, Feb. 16, 2024).
As distinct from Palforzia, which gradually desensitizes a person to a food allergen, omalizumab interferes with the allergic reaction. It does not cure a food allergy, however. In the study, just over two-thirds of patients were able to eat at least 600 mg of peanut protein (equivalent to 2.5 peanuts) without having “moderate to severe allergic symptoms,” says the FDA. Comparable results occurred with eggs and milk. While not a cure for food allergy, the new drug approach may reduce the risk for severe and dangerous food allergic reactions for some people. Avoidance of allergenic foods is still crucial. The FDA describes this drug as “the first FDA-approved medication to reduce allergic reactions to more than one type of food after accidental exposure.”

Anyone who excludes a food group such as dairy or grains due to allergy or food intolerance runs the risk of compromised nutrient intake.
For example, a person who avoids milk due to allergy could be at risk of inadequate intake of calcium, vitamin D, protein, and other nutrients. Children who have cow’s milk allergy commonly have a deficiency of calcium, according to Gargano et al. (2021).
A Registered Dietitian working with those who have food allergies can help identify nutrient shortfalls in an elimination or avoidance diet, recommending ways to replace these nutrients, say Gargano et al. (2021). Nutrition consultation is especially important for young children, they suggest—especially for those with multiple sensitivities. Nutrient demands for growth are high, and it is especially important to find safe substitutes for high-protein foods such as milk or eggs, they note. Research has demonstrated the occurrence of kwashiorkor (severe protein malnutrition) in children who were on elimination diets, note Gargano et al. Ongoing consultation is advisable, they say, because “tolerance can be different for each food and can change over time.”
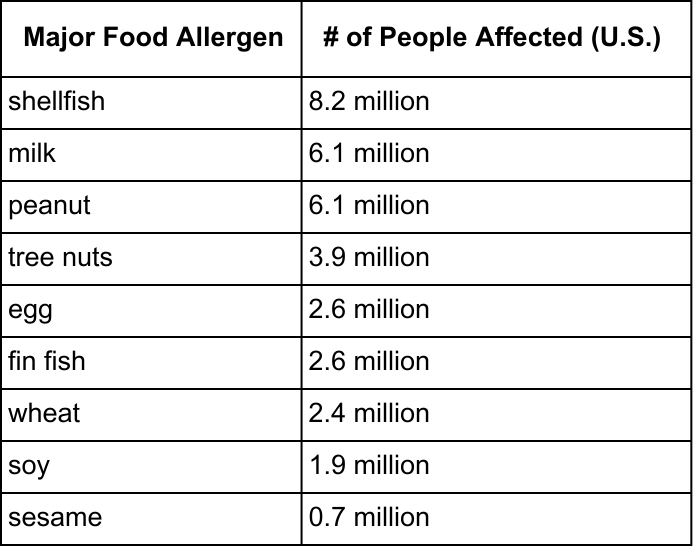
Many foods are known to be implicated in food allergies. However, nine foods cause the majority of cases (FDA, 2023).
The Food Allergen Labeling and Consumer Protection Act (FALCPA) was passed in 2004 to protect consumers by requiring major food allergens to be declared on food labels. At that time, experts said that 90% of food allergies and serious allergic reactions in the U.S. were associated with eight food allergens: milk, eggs, fin fish, crustacean shellfish, tree nuts, peanuts, wheat, and soybeans. Effective January 1, 2023, a ninth major food allergen was recognized as part of the Food Allergy Safety, Treatment, Education, and Research (FASTER) Act: sesame.
The FARE ranks prevalence as follows (see chart on left)
Two out of five children with food allergies are allergic to more than one food, they note. For cow’s milk allergy in childhood, 19% of cases resolve by age 4, and 79% resolve by age 16 (Iglesias et al., 2024). Furthermore, research indicates that 89% of egg allergies resolve by age 6, they note. Peanut and tree nut allergies have higher levels of persistence.
Which allergens are most responsible for anaphylactic events varies by global geography. In The U.S., peanuts are responsible for the highest number, followed by tree nuts.
Besides the big nine food allergens addressed in food labeling law, there are more than 160 foods that can cause allergy for some people, according to the FDA (2023). There are also some food ingredients that cause “nonallergic hypersensitivity reactions” in some people, they add.
Sometimes, people who believe they have a food allergy may actually have an intolerance, which is different, explains the AAAAI (Food Intolerance vs. Food Allergy, 2023). They explain food intolerance as a food sensitivity that “occurs when a person has difficulty digesting a particular food”. An intolerance is not an immune system response. The definition of “intolerance” includes “metabolic, toxic, pharmacologic, and undefined mechanisms,” according to Gargano and colleagues (2021).
Symptoms can be intestinal gas, abdominal pain, or diarrhea. Unlike food allergy, an intolerance is not an immunologic reaction.
Up to about one in five people may have some food intolerance, according to Tuck and colleagues (2019). Overall, the prevalence of food intolerances is unknown, suggest Gargano and colleagues. This is because there is a lack of controlled research and a lack of diagnostic procedures for confirming many food intolerances. There is no reliable way to conduct blood tests for food intolerances, note Tuck and colleagues. A common approach is trial-and-error.
Some food intolerance tests are marketed to consumers, such as IgG tests, says the AAAAI (Jan. 10, 2023). Test promotions may claim that “removal of foods with high IgG levels can lead to improvement in multiple symptoms,” but this approach is not backed by evidence, they note.
Difficulty digesting a food could be due to a lack of specific enzymes, as in lack of the lactase enzyme causing lactose intolerance associated with consuming milk and dairy products. About 36% of Americans have lactose intolerance, according to the National Institute of Diabetes and Digestive and Kidney Diseases (2018).
Lactose intolerance is least common among people with European ancestry. In the U.S., demographics that are most likely to have lactose intolerance are African Americans, American Indians. Asian Americans, and Hispanics/Latinos, they add.
With an intolerance, it may not be necessary to entirely eliminate a food from the diet. In lactose intolerance, for example, the body may be producing some lactase—just not enough.
A number of “nonallergic sensitivity reactions” may exist among sensitive individuals, according to the FDA (2023). A popular example is gluten, a type of protein found in wheat, barley, rye, and other grains. In the case of celiac disease, eating gluten leads to an immune response that damages the lining of the small intestine. Many people who do not have a diagnosis of celiac disease or wheat allergy believe they are sensitive to gluten, with associated symptoms of abdominal pain, bloating, diarrhea, fatigue, headache and other findings. This condition is called nonceliac gluten sensitivity. Because there is no test for it, experts can only estimate the condition affects somewhere between 0.6 and 13% of people worldwide (Catassi et al, 2023).
While the gluten protein may cause this condition, researchers have been focusing on other explanations involving other components of wheat, explain Catassi and colleagues. One observation is that wheat contains high amounts of fructans, which fall into the classification of Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs). Fructans are a type of carbohydrate composed of fructose (sugar) molecules. FODMAPs are a large category of foods that has been demonstrated to elicit many of the same gastrointestinal symptoms. For affected people, certain high-FODMAP foods are culprits in food intolerance. A significant body of research has demonstrated the value of a low FODMAP diet in treatment of irritable bowel syndrome.
Another wheat component, amylase/trypsin inhibitors (ATIs) also seem to cause adverse effects for some people. Nonceliac gluten sensitivity condition may also be associated with autoimmune diseases, but cause-and-effect are unclear. Based on these areas of research, experts prefer to use the term, “nonceliac wheat sensitivity”.
Other food components that may not be tolerated by some people include histamines and sulfites (Gargano et al., 2021). The FDA also mentions FD&C Yellow No. 5, as well as the color additive carmine, which is made from insects, as ingredients that can trigger sensitivities for some people. Currently, the FDA requires label declaration on those color agents, as well as of sulfites.
Only a food allergy introduces a specific protein into the immune system, causing an immune response. While an intolerance may cause uncomfortable symptoms, an allergy can cause potentially life-threatening reactions, notes AAAAI. Another distinction between food allergy and food intolerance is that a food allergenic response can happen even at very small doses of the offending food allergen. In contrast, a food intolerance is typically dose-dependent; the greater quantity of a food consumers, the more severe the symptoms are (Gargano et al.).

Oral Allergy Syndrome, also called Pollen Food Allergy Syndrome, occurs because of cross-reactivity, explains the AAAAI (Oral Allergy Syndrome, 2024). “Being allergic to a food may also result in being allergic to a similar protein found in something else” as the body “confuses” the proteins with each other. Anyone who is allergic to certain pollens may also react to certain foods. This may be somewhat seasonal, with reactions occurring when particular pollen counts are highest.
Itching and swelling of the mouth, face, lips, tongue, and throat would be common reactions in oral allergy syndrome. These could occur immediately or up to an hour after eating a raw fruit or vegetable. Only rarely can this cause an anaphylactic rection, they note.
Here are some examples:
The AAAAI advice for managing oral allergy syndrome is to:
When an oral reaction to nuts appears, the AAAAI recommends consulting with an allergist because this could be indicative of a more serious allergy. A consultation is also warranted for a person who has hives, vomiting, or difficulty breathing, they suggest.
A condition called Food-Dependent Exercise-Induced Anaphylaxis (FDEIA) can trigger serious symptoms affecting the skin, gastrointestinal tract, and/or respiratory systems. It can cause anaphylaxis (Gargano et al., 2021). The AAAAI (2018) explains the condition as a type of food allergy that only manifests in the presence of exercise. How this occurs is not well understood.
FDEIA was first described in 1979 in a case of a person who had serious shellfish allergy—but only when exercising. A person who has this condition can ordinarily consume the allergenic food with no effect, but can become seriously ill or experience anaphylaxis when eating the food up to four hours before physical activity, say Gargano et al. Many foods can be allergenic culprits. Wheat is the most common FDEIA trigger in children, especially in teenage males. For adults, “the most common allergens are seafood, peanuts, and tree nuts,” says AAAAI.
Exercise is considered a cofactor in triggering the allergic response. Cofactors are “elements that lower the threshold to develop food-induced allergic symptoms,” explain Iglesia et al. (2024). Other cofactors that can influence whether a person develops an allergic response are current illness, fever, alcohol consumption, menstruation, aspirin, and other non-steroidal anti-inflammatory drugs,” they explain.
Another condition related to food allergy is called Eosinophilic Gastrointestinal (GI) disease. This often first appears in infancy but can be diagnosed at any age. The most common site is the esophagus. In pediatric patients, the condition is typically associated with failure to thrive. In adults, it often presents as dysphagia (difficulty swallowing) and gastroesophageal reflux disease (GERD).
Other parts of the GI tract can (less commonly) be affected. For non-esophageal versions of the condition, “Abdominal pain was the main gastrointestinal symptom in children (94%), while diarrhea was the most prevalent symptom (100%) in adults,” explains AAAAI (May 1, 2023).
This condition is not strictly a food allergy, notes AAAAI. Instead, it is an “allergic/immune condition of the esophagus” (or other part of the GI system). A type of white blood cells called eosinophils “can release substances into surrounding tissues that cause inflammation”. An allergenic response to environmental factors or to food compounds the problem. For reasons unknown, the condition is on the rise.
Many people who experience an eosinophilic GI condition also have one or more allergic disorders. “Environmental allergies to substances such as pollens, animals, dust mites and molds possibly play a role,” says AAAAI. Some people find the condition is worse when pollen counts are high. However, for most people with eosinophilic disease affecting the esophagus, AAAAI says, “Immune reactions to foods are the main cause.” Commonly involved foods are dairy products, wheat, egg, and soy.
Food connections are hard to pin down, though, because the allergic reactions are delayed rather than immediate. Common allergy tests, such as skin tests and blood tests for IgEs are not reliable for this condition, the AAAAI notes. Once the offending food(s) is/are identified and removed from the diet, the condition usually resolves within a few weeks. Other treatments are often used as well.

A recently discovered form of food allergy is alpha gal allergy, which is a potentially life-threatening allergic response that can occur after eating red meat or products made from gelatin or other red meat components (CDC, Oct. 27, 2023). “Alpha-gal” is the short name for a specific sugar molecule found in most mammals. This is an unusual form of food allergy because the body is reacting to a carbohydrate rather than a protein.
Allergic symptoms arise 2-6 hours after eating the food, often awakening the person at night. Symptoms can range from hives and rash to severe stomach pain, dizziness, and difficulty breathing. This allergy is associated with being bitten by the Lone Star tick (and possibly other ticks), which pass the alpha-gal to a person through their bite. “People with alpha gal allergy should avoid beef, lamb, pork and venison,” says AAAAI (Food Allergy, 2024). They may also need to work with a health professional to identify other sources of the allergen.
“Food allergy prevalence appears to be rising and has become a serious public health issue,” according to the National Institute of Allergy and Infectious Diseases (March 8, 2023). FARE (Facts and Statistics, 2024) cites these public health stats:
For children, racial and ethnic disparities are evident. “Black, non-Hispanic children are more likely to have a food allergy (7.6%) compared to Hispanic (5%) and White, non-Hispanic (5.3%) children” (CDC, Jan. 26, 2023). For adults, the figures are similar: “Black, Non-Hispanic adults are more likely to have a food allergy (8.5%) compared to Hispanic (4.4%); White, non-Hispanic (6.2%), and Asian, non-Hispanic (4.5%) adults.”
Reasons for the disparities are not definitively understood. Jones and colleagues (2022) note that a major study on food allergy found that “African American children with an allergy to peanut, milk or egg were less likely to be introduced to respective allergens early in infancy compared with white children.” A higher prevalence of asthma may also be related. “Those from disadvantaged socio‐economic groups are more likely to be exposed to asthma environmental triggers,” say the authors. The explanation is likely multi-factorial, involving “environment interaction, behavioral and cultural elements,” they hypothesize.
As an example of how socioeconomic and racial disparities may develop, Thivalapill et al. (2022) note that African American children have double the risk of allergy to shellfish, as compared with White children. The connection, they say, is sensitization that can occur through exposure to cockroaches in living environments. This happens because of protein similarities between the cockroaches and shellfish.

The FDA plays a major role in protecting consumers from food allergy symptoms (FDA, 2023). They:

The Food Allergen Labeling and Consumer Protection Act (FALCPA) requires that “the allergen's food source must be declared at least once on the food label in one of two ways,” says the FDA (2023). One option is translation of ingredients that might not be obvious as these allergens. For instance, whey contains milk protein, so an ingredient list would say: whey (milk). Another option a “contains” statement, e.g., “Contains wheat, milk, and soy.”
The law also requires that the label declare the food source of all major food allergens used to make the food. For example, a label must name the type of tree nut (e.g., almonds, pecans, walnuts); the species of fish (e.g., bass, flounder, cod); the species of shellfish (e.g., crab, lobster, shrimp).
Although not required by law, some manufacturers use advisory statements such as “may contain [allergen] or “produced in a facility that also uses [allergen].”
Consumers with allergies should be aware of how the major allergens are defined for the purpose of allergen labeling,” cautions the FDA (2023). For example, for labeling purposes, “eggs” refers to the protein in chicken eggs. Yet similar proteins may appear in eggs from other birds. Similarly, “milk” refers to cow’s milk. Milk from goats, sheep, or other mammals would not bear an allergen warning.
“FALCPA's labeling requirements extend to retail and food-service establishments that package, label, and offer products for human consumption. However, FALCPA's labeling requirements do not apply to foods that are placed in a wrapper or container (such as paper or a box for a sandwich) following a customer’s order at the point of purchase,” says the FDA.

As distinct from past advice, the current scientific consensus about introducing potential allergens emphasizes early introduction of foods. This is based on a large body of research, which Iglesia et al. (2024) explain has “demonstrated that timely and consistent feeding of allergenic foods such as peanuts and eggs during infancy and into early childhood is an effective primary prevention strategy against the development of food allergy.” This is particularly important for infants who have eczema, because they are considered at higher risk of developing food allergy.
The bulk of research on this topic involves peanuts, eggs, and cow’s milk (Abrams et al., 2023). A one-time introduction is likely to be insufficient. Based on research, experts also emphasize that regular consumption of the food is important for success, explain Abrams et al. However, an exact protocol for dose and frequency has not been confirmed.
For eggs, preparation methods are also important because cooking can denature potentially allergenic proteins. Some studies with egg introduction to infants have reached varying conclusions, and the authors attribute discrepancies to differences in cooking methods. A “least allergenic” form of eggs, they say, is in a baked preparation, such as muffins. Cooked eggs, such as hard-boiled, scrambled, or omelet dishes have stronger allergenic effects and are thus more useful for preventing food allergy down the line.
The AAAAI recommends that eggs and peanuts be introduced to infants at approximately 6 months of age. For infants aged 4-6 months who have a known egg allergy and/or severe eczema, some medical professional bodies, such as the American Academy of Pediatrics, recommend skin prick testing or IgE testing up front (Abrams et al.).
Some evidence suggests that as a general principle, dietary diversity early in life may be protective against development of food allergies, including foods beyond those that have been the focus of research (Abrams et al.). The authors advocate for “consistent positive messaging” about “the safety and benefits of introducing allergenic foods during early infancy”.
Foodservice managers need to be aware that most fatal food allergy reactions are triggered by food consumed outside the home (FARE, Facts and Statistics, 2024).
The FDA Food Code (FDA, 2022), which serves as a model for food sanitation guidance across the nation, defines a number of best practices for foodservice, specifies the importance of ensuring that employees are trained in food allergy. An FDA suggested training outline covers:
It is crucial the foodservice managers are “aware of the serious nature of food allergies, including allergic reactions, anaphylaxis, and death,” they explain. Managers should also understand food allergen ingredient identities and labeling, as well as methods for avoiding cross-contact during food preparation and service.
Cross-contact is defined as “the inadvertent introduction of an allergen into a product that would not intentionally contain that allergen as an ingredient” (FDA). Similar to the practice of preventing cross-contamination, preventing cross-contact requires cleaning and sanitizing contact surfaces of equipment and utensils that have contacted major food allergens prior to contacting other foods.
Menu transparency is imperative, as guests who have food allergies may be reviewing descriptions when choosing foods. Allergens not identified in menu descriptions can cause mistakes.
Foodservice managers should also be aware of their obligation to provide appropriate accommodations for guests who have food allergies. “Food allergy limits a major life activity and may qualify an individual for protection under the Americans with Disabilities Act of 1990 (ADA) and Section 504 of the Rehabilitation Act of 1973,” says the FDA (2023).
Extensive resources are available for developing comprehensive policies and procedures related to food allergies. For example, the National Restaurant Association offers ServSafe Allergens training. FARE (2024) resources include guidelines for creating an inclusive environment, a sample dining audit, and a course on responding to anaphylaxis. A book from the National Academies Press (2017), a free download, provides extensive resources for foodservice policies and procedures. The CDC (2013) provides a comprehensive guide for school foodservice.
Keeping guests who have food allergies safe is a multi-pronged effort involving every employee, and often other stakeholders, too. Investing the time to develop effective policies procedures, training staff, and communicating well with guests all play a role in ensuring a safe foodservice experience.

Food allergy affects approximately 8% of children and 11% of adults in the U.S. A majority (but not all) of allergies relate to nine foods, which are identified on food labels in accordance with the FALCPA Act. Symptoms of food allergy can range from mild to severe or life-threatening. The incidence of food allergy in the U.S. is rising.
Some mysteries about food allergy persist, such as why some people and not others become sensitized to a food, or how a person who has IgE antibodies to a food can escape having allergic reactions.
Development of food allergy can potentially be reduced by introducing foods such as eggs and peanuts in infancy. There is no cure for food allergy. However, new treatments may reduce the likelihood of severe reactions.
In foodservice, controls must be embedded into policies, procedures, training, and communications in order to accommodate everyone and keep guests safe.
Abrams, E. et al. (Oct. 11, 2023). Updates in Food Allergy Prevention in Children. Pediatrics.
American Academy of Allergy Asthma & Immunology (AAAAI). (May 1, 2023). Eosinophilic Esophagitis. https://www.aaaai.org/
American Academy of Allergy Asthma & Immunology (AAAAI). (accessed Mar. 2, 2024). Food Allergy. https://www.aaaai.org/
American Academy of Allergy Asthma & Immunology (AAAAI). (Dec. 27, 2023). Food Intolerance Versus Food Allergy. https://www.aaaai.org/
American Academy of Allergy Asthma & Immunology (AAAAI). (Dec. 27, 2023). Food Protein-Induced Enterocolitis Syndrome (FPIES). https Updates in Food Allergy Prevention in Children.://www.aaaai.org/
American Academy of Allergy Asthma & Immunology (AAAAI). (Jan. 10, 2023). The Myth of IgG Food Panel Testing. https://www.aaaai.org/
American Academy of Allergy Asthma & Immunology (AAAAI). (accessed Mar. 2, 2024). Oral Allergy Syndrome (OAS). https://www.aaaai.org/
American Academy of Allergy Asthma & Immunology (AAAAI). (Feb. 28, 2018). Wheat dependent, exercise induced anaphylaxis, an evolving concept. https://www.aaaai.org/
CDC. (Oct. 27, 2023). Alpha-gal Syndrome. https://www.cdc.gov/ticks/alpha-gal/index.html
CDC. (Jan. 26, 2023). More Than a Quarter of U.S. Adults and Children Have at Least One Allergy. Press release.
CDC. (2013). Voluntary Guidelines for Managing Food Allergies in Schools and Early Care and Education Programs.
Catassi, C. et al. (Sept. 2023). Nonceliac Gluten Sensitivity. Curr Opin Clin Nutr Metab Care.
FARE. (accessed Mar. 2, 2024). Facts and Statistics. https://www.foodallergy.org/
FARE. (accessed Mar. 1, 2024). Living with Food Allergies [resources for college and university foodservice]. https://www.foodallergy.org/
FDA. (2022). 2022 Food Code. https://www.fda.gov/
FDA. (Jan. 31, 2020). FDA Approves First Drug for Treatment of Peanut Allergy for Children. News release.
FDA. (Feb. 16, 2024). FDA Approves First Medication to Help Reduce Allergic Reactions to Multiple Foods After Accidental Exposure. News release.
FDA. (Jan. 10, 2023). Food Allergies. https://www.fda.gov/
Gargano et al. (May 13, 2021). Food Allergy and Intolerance: A Narrative Review on Nutritional Concerns. Nutrients.
Iglesia, E. et al. (Feb. 13, 2024). Management of Food Allergies and Food-Related Anaphylaxis. JAMA.
Jones, C. et al. (May 2022). Burden of allergic disease among ethnic minority groups in high‐income countries. Clinical and Experimental Allergy.
National Academies Press. (2017). Finding a Path to Safety in Food Allergy: Assessment of the Global Burden, Causes, Prevention, Management, and Public Policy. https://nap.nationalacademies.org/download/23658
National Institute of Allergy and Infectious Diseases. (Feb. 25, 2024). Antibody Reduces Allergic Reactions to Multiple Foods in NIH Trial. News release. https://www.niaid.nih.gov/
National Institute of Allergy and Infectious Diseases. (Mar. 8, 2023). Food Allergy. https://www.niaid.nih.gov/diseases-conditions/food-allergy
National Institute of Diabetes and Digestive and Kidney Diseases. (2018). Definition & Facts for Lactose Intolerance. https://www.niddk.nih.gov/
National Restaurant Association. (accessed March 3, 2024). ServSafe Allergens. https://www.servsafe.com/ServSafe-Allergens
Reardon, S. (Feb. 26, 2024). ‘Breakthrough’ Allergy Drug: Injection Protects Against Severe Food Reactions. Nature.
Thivalapill, N. et al. (Aug. 4, 2022). Sensitization to House Dust Mite and Cockroach May Mediate the Racial Difference in Shellfish Allergy. Pediatric Allergy and Immunology.
Tuck, C. et al. (July 22, 2019). Food Intolerances. Nutrients.
USDA. (accessed Mar. 2, 2024). Food Allergies. https://www.fsis.usda.gov/
Select the correct answer for each question.
1. Immediate symptoms of swelling of the throat and vocal cords, difficulty breathing, dizziness, and/or loss of consciousness are symptoms of
Select the correct answer for each question.
2. Which food allergen was recognized by the Food Allergy Safety, Treatment, Education, and Research (FASTER) Act effective January 1, 2023?
Select the correct answer for each question.
3. A food intolerance occurs when a person has
Select the correct answer for each question.
4. The inadvertent introduction of an allergen into a product that would not intentionally contain that allergen as an ingredient is the definition of
Course complete!
Your Score: out of 4 correct.
You did it! Click the button below to download your certificate of completion for this course. Keep it for your records. To make it easy on you, we have made the certificate fillable.
Download CertificateDid you like the course you completed? Do you have any feedback or suggestions for future courses? We can’t wait to review your feedback!
Complete Course EvaluationIf you would like to submit your evaluation and comments to the Commission on Dietetic Registration, you may do so at QualityCPE@eatright.org.